Contents
Moraxella catarrhalis is a gram-negative diplococcus that resembles non-pathogenic Neisseria both morphologically and metabolically.
Microbiology
Gram-negative diplococcus that produces nonhemolytic, round, opaque colonies on blood agar.
- Bacterial culture: Colonies of M. catarrhalis resemble commensal Neisseria that are present in the normal human upper airway flora. M. catarrhalis colonies can be slid along the agar surface without disruption; this is termed the “hockey puck sign.”
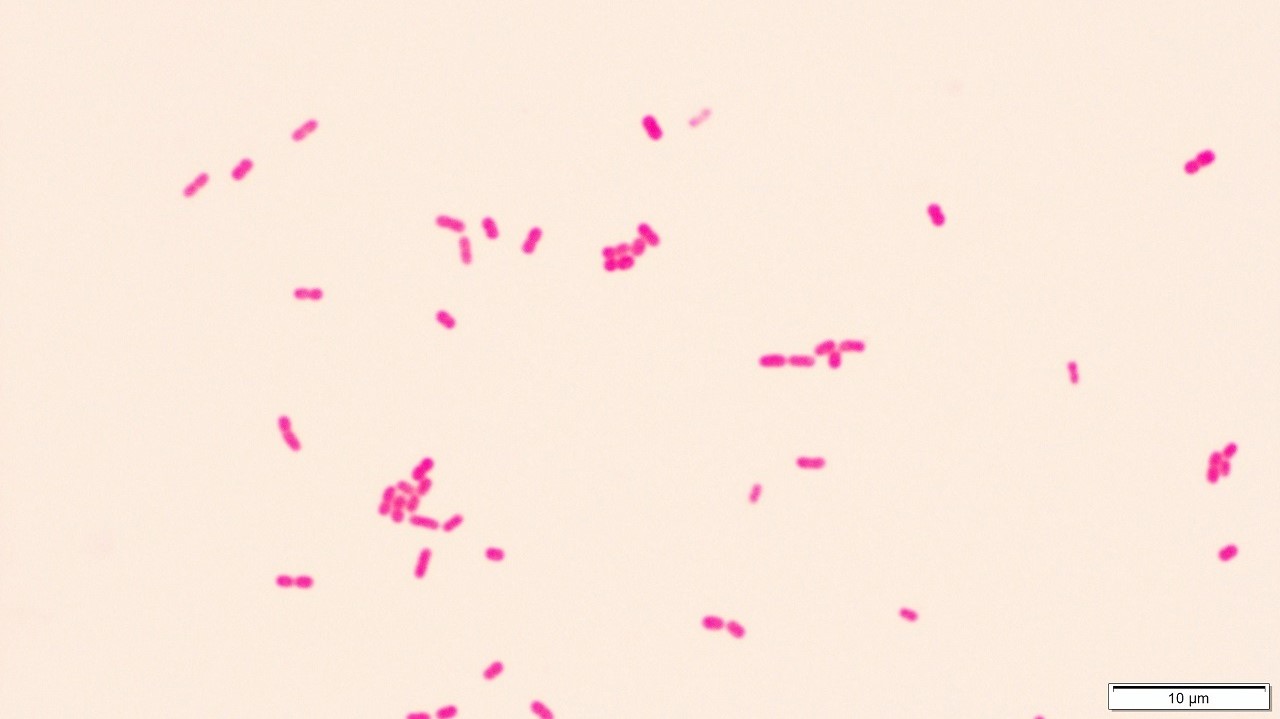
- Gram-stained smears: Gram-negative diplococci as the predominant bacterial form, with bacteria typically observed intracellularly within neutrophils

(A) Sputum Gram stain showed neutrophils and Gram-negative diplococci resembling Moraxella sp or Neisseria sp. (B) The colonies were able to be slid across the agar surface without disruption, a feature known as the ‘hockey puck sign’. | Kano, Y. (2021). Hockey puck sign: Identifying Moraxella catarrhalis. BMJ Case Reports CP, 14(4), e243677. https://doi.org/10.1136/bcr-2021-243677 
Fried egg appearance of Moraxella growing on trypticase soy agar supplemented with 5% sheep blood. The colonies were magnified by 20× | LaCroce, S. J., Wilson, M. N., Romanowski, J. E., Newman, J. D., Jhanji, V., Shanks, R. M. Q., & Kowalski, R. P. (2019). Moraxella nonliquefaciens and M. osloensis Are Important Moraxella Species That Cause Ocular Infections. Microorganisms, 7(6), 163. https://doi.org/10.3390/microorganisms7060163
Biochemical tests:
To distinguish M. catarrhalis from Neisseria. Kits that use these biochemical reactions are commercially available.
- M. catarrhalis produce oxidase, catalase, and DNAse (detected using DNAse test agar with methyl green); reduce nitrate and nitrite; and hydrolyze tributyrin.
- M. catarrhalis does not ferment carbohydrates.
Pathogenesis
It is considered to be a part of the normal oropharyngeal flora, but can become pathogenic causing severe meningitis and endocarditis, as well as sinusitis, otitis media, and lower respiratory tract infections.
Acute otitis media:
Approximately 80% of children experience an episode of otitis media by the age of 3 years. Otitis media is the most common bacterial infectious disease in childhood and the most common reason for which children receive antibiotics. Streptococcus pneumoniae, nontypeable Haemophilus influenzae, and M. catarrhalis (15-20%) are the predominant causes of acute otitis media.
Chronic obstructive pulmonary disease (COPD):
Course characterized by intermittent exacerbations which are associated with lost work time, emergency room visits, hospital admissions, respiratory failure, and sometimes death. Approximately one-half of exacerbations are caused by bacterial infection, with the remainder being caused by viral infection and noninfectious causes. The clinical features of an exacerbation due to M. catarrhalis are similar to those of exacerbations due to other pathogenic bacteria, including H. influenzae and S. pneumoniae. The cardinal symptoms of COPD exacerbations are increased sputum production, sputum purulence, and dyspnea, compared with baseline symptoms. Other features may include fever and fatigue.

Other infections:
- Bacterial sinusitis: Occurs after a small percentage of viral upper respiratory tract infections. M. catarrhalis is responsible for ∼20% of cases of acute bacterial sinusitis in children and a smaller proportion of cases in adults and is clinically indistinguishable from that caused by S. pneumoniae or H. influenzae.
- Invasive infections (bacteremia, pneumonia): Pneumonia due to M. catarrhalis occurs infrequently but is well described in elderly persons, especially in those with underlying cardiopulmonary disease. M. catarrhalis rarely causes bacteremic illness.
Management
More than 90% of M. catarrhalis produce a β-lactamase and are, thus, resistant to ampicillin.
Oral antibiotic therapy:
Treatment of otitis media in children and exacerbations of COPD in adults, the 2 most common infectious diseases caused by M catarrhalis, is generally empirical. Therefore, antimicrobial agents that are active against S. pneumoniae and H. influenzae, in addition to M. catarrhalis, are usually administered.
- Amoxiclav
- Extended spectrum cephalosporins: Cefixime, cefpodixime, defaclor, loracarbef, cefuroxime
- Macrolides: Azithromycin, clarithromycin
- Trimethoprim-sulfamethoxazole
- Tetracyclines
- Fluoroquinolones