Contents
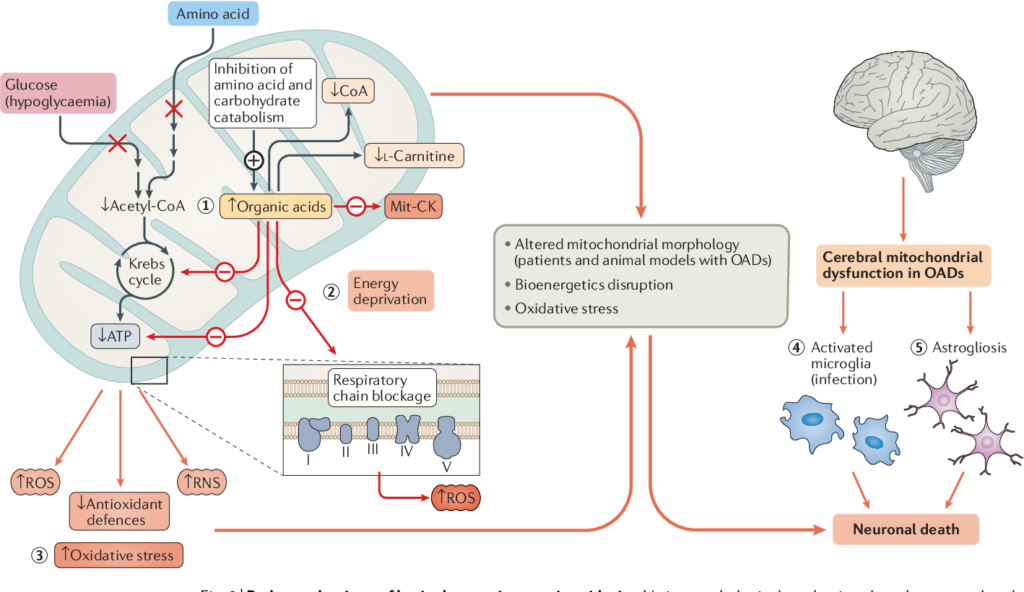
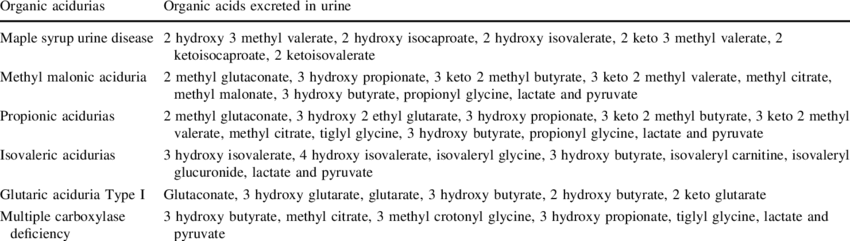
Inborn errors of metabolism (IEM) affecting enzymes and/or transport proteins required for catabolism of amino acids (AAs), lipids, or carbohydrates lead to pathologic buildup of upstream substrates/metabolites resulting in the clinical manifestations of organic acid disorders (OADs), also known as organic acidemias or acidurias.
An increase in plasma ammonia to toxic levels is often a key feature of metabolic decompensation, which needs to be addressed promptly since it can lead to life-threatening neurological complications.
- All organic acidurias are inherited as autosomal recessive conditions.

Classification
Common ‘Classic’ OAs:
Refer to the most common inborn errors of branched chain AA (BCAA) catabolism These OAs usually result in hyperammonaemia during acute metabolic decompensation
- Propionic acidemia (PA)
- Methylmalonic acidemia (MMA)
- Isovaleric acidemia (IVA)
- Maple syrup urine disease (MSUD)

Biochemical basis:

Uncommon OAs:

“Cerebral” OAs:
This group of organic acid disorders presents exclusively with neurological symptoms. As a group these “cerebral” organic acid disorders appear to remain often undiagnosed and their true incidence is much less well-known than that of the “classical” organic acid disorders.
- Glutaryl-CoA dehydrogenase deficiency (glutaric aciduria type I)
- Succinic semialdehyde dehydrogenase deficiency (4-hydroxybutyric aciduria)
- Mevalonic aciduria
- N-acetylaspartic aciduria (Canavan disease)
- L-2-hydroxyglutaric aciduria
Neurological manifestations are very common and can be the leading and/or presenting feature in organic acid disorders, sometimes in the absence of metabolic derangement. Review of the time course and presentation of neurological disease in organic acid disorders reveals characteristic clinical findings of ataxia, myoclonus, extrapyramidal symptoms, metabolic stroke and megalencephaly.
Presentation
The development of an acute, life-threatening illness in a previously apparently healthy neonate is a strong indicator of an inherited metabolic disorder.
Initial presentation: VOMIT (valine, odd chain fatty acids, methionine, isoleucine, and threonine)
Characteristic biochemical finding of propiogenic essential AA (valine, methionine, isoleucine, and threonine) and odd chain fatty acids imbalance with initial clinical findings of vomiting.
- Acute attacks triggered by conditions that increase catabolism:
- Neonates: Normal diet of breast milk or formula + postpartum catabolism
- Beyond neonates: Fasting, vomiting or febrile infections
Established disease:
Major clinical features are developmental delay/mental retardation, seizures, lethargy, coma, hypotonia, vomiting, failure to thrive, hepatomegaly, respiratory distress, and cardiac dysfunction. The symptoms worsen in the absence of supporting care and can proceed to coma/death. A diagnosis in the first 24–48 h is vital and can prevent chronic sequel including physical/mental retardation.
- Neonates (2–7 days after birth): Poor feeding, vomiting, dehydration, lethargy, tachycardia and hypothermia
- If left untreated, can quickly progress to respiratory distress, coma and death
- Beyond neonates: Delays in development, failure to thrive, altered mental state, abnormal tone, seizures and motor dysfunction
Biochemical features:
Organic acidurias generally present with hyperammonemia and high anion gap metabolic acidosis. Additional biochemical features include hypoglycemia, ketonuria etc.
- Severe and persistent metabolic acidosis of unexplained origin
- Elevated anion gap
- Severe neurologic manifestations: Encephalopathy or seizures
Other signs and symptoms of acute/chronic decompensation:
- Weight loss (often seen in newborns)
- Bone-marrow suppression (PA and MMA)
- Characteristic ‘sweaty feet’ odour (IVA)
Diagnosis
Screening tests:
- DNPH test (Di nitro phenyl hydrazine test)
- Thin layer chromatography
Confirmatory tests:
Most of these tests are very expensive and thus not routinely performed
- HPLC
- GC/MS
- Tandem mass spectrometry
- Enzyme assays/DNA analysis
- High-field proton NMR

Management
Treatment strategies also involve cofactor/vitamin utilization to aid specific pathways and disorder management. Optimal metabolic control and regular monitoring is key to long-term management and prevention of morbidity, disability and mortality.
Nutritional management:
Goal of nutritional therapy is to provide all essential nutrients to promote physical and mental development. Synthetic amino acid based formulas should provide approximately 50% of daily protein requirement.
- Amino acid based formulas: Provide energy, nitrogen, vitamins and minerals which can promote anabolism and growth
- Restriction of offending dietary precursor amino acid
Fastingto be avoided- L-Carnitine (as well as biotin): As secondary carnitine deficiency is common and carnitine promotes urinary excretion of urinary organic acid esters
- Metronidazole: Reduce endogenous gut propionate
Acute management:
Aim is to correct hyperammonaemia in organic acidaemias
- Dialysis
- Correction of fluid and electrolyte imbalances
- Correction of acidosis as well as maintenance of cerebral function with adequate perfusion
- Oxygen and glucose as the case demands

One reply on “Organic acid disorders (OADs)”
[…] Organic acid disorders (OADs): […]